Tissue Nematodes
420 likes | 1.35k Vues
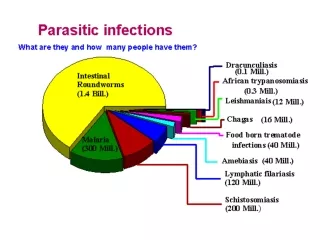
Tissue Nematodes. II BPT. Classification – Tissue Nematodes. Lymphatic. Wuchereria bancrofti. Brugia malayi. Brugia timori. Subcutaneous. Loa loa (african eye worm). Onchocerca volvulus (blinding filaria). Dracunculus medinensis (thread worm). Conjunctiva . Loa loa.

Tissue Nematodes
E N D
Presentation Transcript
Tissue Nematodes II BPT
Classification – Tissue Nematodes Lymphatic Wuchereria bancrofti Brugia malayi Brugia timori Subcutaneous Loa loa (african eye worm) Onchocerca volvulus (blinding filaria) Dracunculus medinensis (thread worm) Conjunctiva Loa loa
Wuchereria bancrofti (Filarial worm) Definitive host Man Intermediate host Female Culex, Aedes or Anopheles mosquito Infective form Third stage larva Mode of transmission Inoculation – bite of mosquito Site of localization Lymphatics / lymph nodes of man
Clinical features • Infection - Wuchereriasis/ Lymphatic filarisis/ Bancroftian filariasis • Pathogenic states are produced only by adult worm (living/ dead) – classical filariasis Occult filariasis – lesions produced by microfilaria • Clinical states in classical filariasis can be classified as: • Asymptomatic ( in endemic areas) • Inflammatory – lymphadenitis, lymphangitis, fever, lymphoedema • Obstructive – elephantiasis, lymphangiovarix, chyluria, hydrocele • Tropical pulmonary eosinophilia
Obstructive stage • Lymphatic obstruction – occurs with the death of worms • Causes of obstruction – • Blocking of lumen by dead worms • Excessive proliferation & thickening of walls of lymphatic vessels • Fibrosis of lymphatic vessels
Consequences of Lymphatic Obstruction • Elephantiasis of organs like leg, scrotum, penis, vagina, breast, arm etc – fibrotic thickening of skin & subcutaneous tissue • Lymphangiovarix – dilatation of afferent lymphatics. • Rupture of Lymphangiovarix into urinary tract – chyluria • Hydrocele
Laboratory diagnosis • Specimen- blood collected at night, preferably capillary blood from ear lobes, chylous urine, hydrocele fluid, exudate from lymphangiovarix • Microscopic examination – wet mount or stained with giemsa: sheathed microfilaria with no nuclei at tail tip
Laboratory diagnosis • Concentration techniques – for capillary blood, venous blood (Knott’s technique) • DEC provocation test – 100 mg of DEC orally, examine peripheral blood smear after 30 to 45 minutes • Serology – using non specific Ags • Passive hemagglutination test • Fluoresecent ab test • ELISA
Treatment DEC (Diethylcarbamazine) – microfilaricidal: 6mg/ kg/day for 2-3 weeks Elevation of the affected limbs, use of elastic bandages & local foot care – reduces symptoms of lymphatic obstruction Surgical treatment of hydrocele Prevention Destruction of mosquitoes Protection against mosquito bites Treatment of carriers
Brugia sps • Two species infect humans : B.malayi & B.timori • Causes lymphatic filariasis • Transmitted by Mansonia & Anopheles species of mosquitoes • Life cycle, pathogenesis, clinical features, diagnosis & treatment – similar to W. bancrofti, with a following differences • Children commonly affected • Rapid development of signs & symptoms • Elephantiasis affect lower extremities • Chyluria & hydrocele rare
Onchocerca volvulus (Blinding filaria – 2nd most common cause of infectious blindness) Definitive host Man Intermediate host Black flies (simulium) Infective form Larva Mode of transmission Inoculation Site of localization Subcutaneous tissue, dermis & eye
Clinical features • Incubation period - 10 to 12 months • Eosinophilia and urticaria. • Nodular and erythematous lesions (Onchocercomata) in the skin and subcutaneous tissue • Photophobia, lacrimation, keratitis and blindness – due to trapping of microfilaria in the cornea, choroid, iris and anterior chambers.
Diagnosis & Treatment • Nodular biopsy – adult worm • Skin snip – unsheathed microfilaria with no nuclei • Treatment – Ivermectin, surgical removal, DEC in non ocular onchocercosis
Loa loa (African eye worm) Definitive host Man Intermediate host Chrysops (deer fly) Infective form Larva Mode of transmission Inoculation Site of localization Subcutaneous & deep connective tissue
Clinical features • Subcutaneous swelling – Calabar or fugitiveswelling, measuring 5 to 10 cm, marked by erythema and angioedema, usually in the extremities • Migrating worm in subconjunctival tissue
Diagnosis & Treatment • Peripheral blood smear - Sheathed microfilaria with nuclei upto rounded tail tip • Isolation of worms from the conjunctiva or subcutaneous biopsy • Treatment - Ivermectin, surgical removal, DEC (effective against adult & microfilaria)
Dracunculus medinensis (Guinea Worm) Adult worms Male 2 to 4 cm Female 70 –120 cms, viviparous Definitive host Human Intermediate host Cyclops Infective form Larva inside Cyclops Mode of transmission Ingestion of water contaminated with cyclops Site of localization Subcutaneous tissue
Clinical Features • Disease – Dracunculosis • Clinical features develop an year after infection following the migration of worm to the subcutaneous tissue of the leg • Blister formation – rupture of blister when in contact with water - ulceration – release of larvae by adult female worm • Secondary bacterial infection of ulcer
Diagnosis & Treatment • Detection of adult worm – when it appears at the surface of skin • Detection of larva – in milky fluid released by worm on exposure to water • Radiology – calcified worm in deeper tissues • Treatment – • Thiabendazole/ Metronodazole – symptomatic relief, easy removal of worm • Gradual extraction of worm by winding of a few cms on a matchstick per day, over 3 to 4 weeks • Surgical excision
Prevention • Provision of safe water supply • Education to discourage people from entering water source • Filtering water through a double folded cloth • Boiling water before drinking • Discouraging the use of step wells