Evolution of Immunization: From Ancient Practices to Modern Vaccines
350 likes | 467 Vues
Explore the milestones in the history of immunization, from variolation in 1700AD to modern vaccines discoveries. Learn about different modes of immunity acquisition, types of vaccines, and attributes of a good vaccine. Understand the response to immunization and the important components of vaccine formulations. Discover the evolution of immunization over centuries.

Evolution of Immunization: From Ancient Practices to Modern Vaccines
E N D
Presentation Transcript
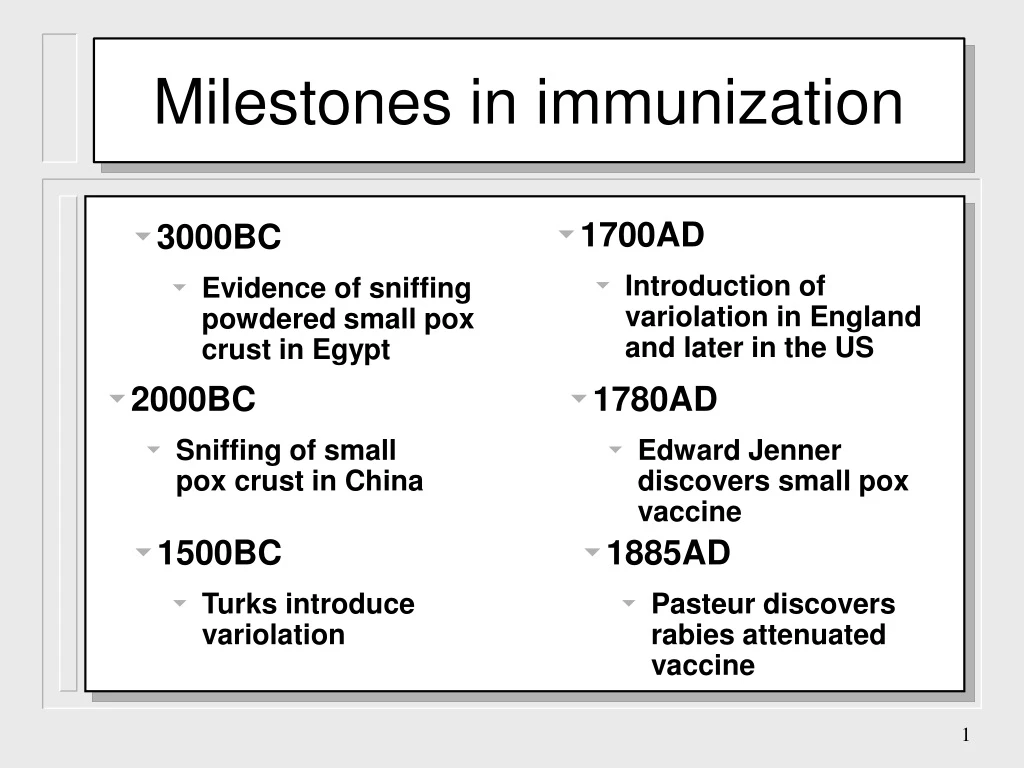
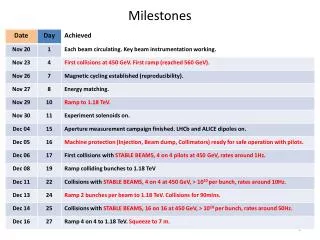
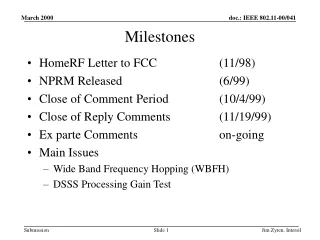
Milestones in immunization • 1700AD • Introduction of variolation in England and later in the US • 3000BC • Evidence of sniffing powdered small pox crust in Egypt • 2000BC • Sniffing of small pox crust in China • 1780AD • Edward Jenner discovers small pox vaccine • 1500BC • Turks introduce variolation • 1885AD • Pasteur discovers rabies attenuated vaccine
Introduction of variolation The wife of the British Ambassador in Turkey, in March 1717 wrote, following the variolation of her son, to a friend in England: “The small pox, so fatal, so general amongst us, is entirely harmless here by the invention of ingrafting….I am patriot enough to bring this invention into fashion in England.
Edward Jenner Discovery of small pox vaccine
Modern era of the vaccine • 1920s • Diphtheria and Tetanus • 1960s • Mumps measles and rubella virus • Sabin polio • 1934 • Pertussis • 1985 • Haemophilus • 1955 • Salk polio • 1990s • Hepatitis and varicella
Acquired Natural resistance Passive Active Artificial Artificial Natural Natural Different modes of acquiring immunity Immunity
Natural Artificial Passive Immunity Placental transfer of IgG Antibodies or immunoglobulins Colostral transfer of IgA Immune cells
disease diphtheria, tetanus human, horse antibody source indication human vericella zoster horse gas gangrene, botulism, snake bite, scorpion sting prophylaxis, therapy immunodeficiencies post-exposure post-exposure human human rabies, prophylaxis hypogamma-globulinemia Passive Immunization
Disadvantages Advantages Advantages and Disadvantages of Passive Immunization no long term protection serum sickness immediate protection risk of hepatitis and Aids graft vs. host disease (cell graft only)
Artificial Natural Active Immunization Attenuated organisms killed organisms exposure to sub-clinical infections sub-cellular fragments toxins others
Live Attenuated Vaccines • hepatitis A • not required in our country • polio* • used in std. schedule measles, mumps & rubella • yellow fever • Military and travelers • Varicella zoster • children with no history of chicken pox • tuberculosis • used at birth
Killed Whole-Organism Vaccines polio • Q fever • population at risk • influenza • elderly and at risk • typhoid, cholera, plague • epidemics and travelers • pertussis • replaced by the acellular vaccine • rabies • post exposure
Microbial Fragment Vaccines • Bordetella. Pertussis • virulence factor protein • Haemophilus influenzae B • protein conjugated polysaccharide • Streptococcus pneumoniae • Polysaccharide mixture • Neisseria meningitidis • polysaccharide
ATTRIBUTES OF A GOOD VACCINE Appropriate immune response Long-term protection Safe Stable Affordable
RESPONSE TO IMMUNIZATION Depends on • Viability of antigen • Total dose • especially killed vaccine • Route and site of administration • Age of recipient • Patient’s condition and immune state • Genetic factors
TYPES OF ANTIGENS 1. Live attenuated (oral polio, BCG, VZV) 2. Killed vaccine (influenza, IPV, Hepatitis A, pertussis) 3. Toxoid (tetanus, diphtheria) 4. Purified (subunit) antigen (Meningococcalvaccine, Haemophilus influenzae vaccine) 5. Recombinant antigen (hepatitis B) 6. DNA vaccines (in investigational phase) 7. Synthetic peptides (in investigational phase)
PURIFIED (SUBUNIT) ANTIGEN • Only parts of pathogen necessary to elicit the immune response are used • Potential toxins are avoided • Need to be conjugated to evoke an adequate T-cell response
POLYSACCHARIDE CONJUGATE VACCINES • Polysaccharide/oligosaccharide of antigen is linked (conjugated) to a protein carrier • increases antibody response and increases of production of memory cells • immunologic response at earlier age • booster effect on subsequent exposure to antigen (via infection /immunization exposure) • E.g. meningococcal vaccine, Haemophilus influenzae type B (Hib) vaccine
Suspending agents e.g. water, saline Preservatives e.g. thiomerosal Stabilisers e.g. sorbitol and hydrolyzed gelatin - MMR Adjuvants e.g. aluminium Salts Other substances which may be present Residuals in the growth medium Antibiotics, e.g. neomycin, streptomycin - IPV, varicella vaccine COMPONENTS OF THE VACCINE FORMULATION • consider these components as well when assessing causality!
COMBINATION VACCINES Diphtheria-tetanus-pertussis (DPT) pertussis component has adjuvant effect for diphtheria and tetanus toxoids Different viruses in one vaccinatione.g. OPV-type 1, 2, 3 polioviruses
ROUTE OF ADMINISTRATION • Should elicit immune response with minimal risk • Deep IM preferable for vaccines with adjuvants (depot effect and less granuloma formation) • SC/intradermal - better for live vaccines • to lessen risk of neurovascular injury but still immunogenic (e.g. BCG)
Vaccines Safety • Checking vials, ampules when applicable, and labels. • Storing vaccine • Checking vaccine and diluent vials/ampules • Checking the vaccine vial monitors
Checking Vials (Ampules) and Labels 1. Label 2. Age of the vaccine (expiration) 3. Signs of contamination 4. Exposure to freezing 5. Exposure to excessive heat
Assessing Contamination • If leaks or cracks are present, discard it • Change in appearance or floating particles are seen, discard it • If submerged in water, discard it • If pierced with used needle, discard it • If vaccine was reconstituted more than 6 hours before, discard it • Vial opened for more than 4 weeks, discard it (WHO)
Assessing Exposure to Freezing • DPT, DT, Td, TT, hepatitis B, diluents and Hib should be discarded if you highly suspect or are certain that they are/were frozen • “Shake taste” DPT, DT, Td and TT (contain aluminum hydroxide adjuvant) when refrigerator log shows subfreezing temperatures. If failed, discard.
Assessing Exposure to Freezing • Hepatitis B and Hib vials should be discarded if frozen or suspected of freezing. The “shake test” doesn’t work for them. • Frozen diluent vials may crack, allowing contamination of the diluent, discard it
Freeze-tag Shelf life is 5 years.
Assessing Exposure to Heat • Vaccine Vial Monitor (VVM) Present: • If VVM inner square is the same color or darker than the outside circle, discard the vial • Vaccine Vial Monitor (VVM) Not Present: • Check temperature log and cold-chain monitoring cards. If exposed to temperatures above 8º C, discard it.
Checking Vaccine Vial Monitors • VVM is a label made of heat-sensitive material, placed on the vial to show cumulative heat exposure over time • VVM reduces waste of vaccine, ensuring that only good vaccine is used
Storage • Fill syringe only when patient is ready to receive an injection • Do not combine partially opened vials • Keep opened vials in the refrigerator in a special box marked “returned”, but remember to discard reconstituted vaccines after 6 hours of reconstitution
Storage Ice Packs in freezing compartment Oral Polio, Measles BCG, DPT, TT, diluent Thermostat Ice packs “Returned box
Checking the Vaccine and Diluent Vials • Before use, check the following: • Is the label still attached to the vial? • Is the right vaccine and right diluent? • Expiration date? • Contamination (discard reconstituted vaccine 6 hours after reconstituted) • Cold sensitive vaccines show no signs of freezing • No signs of heat exposure