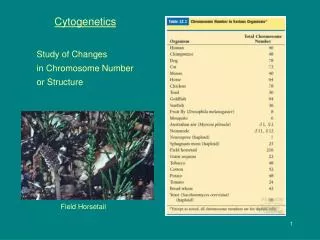
Cytogenetics
680 likes | 1.39k Vues
Cytogenetics. Dr Una Fairbrother. Mitosis. http://www.iupui.edu/%7Ewellsctr/MMIA/htm/animations.htm. Identifying specific chromosomes. Centromere position and arm ratios assist in identifying specific chromosomes Many chromosomes appear identical by these criteria.

Cytogenetics
E N D
Presentation Transcript
Cytogenetics Dr Una Fairbrother
Mitosis • http://www.iupui.edu/%7Ewellsctr/MMIA/htm/animations.htm
Identifying specific chromosomes • Centromere position and arm ratios assist in identifying specific chromosomes • Many chromosomes appear identical by these criteria. • Identifcation revolutionised by dyes producing reproducible patterns of bands
Chromosome banding • Q banding: chromosomes stained with a fluorescent dye such as quinacrine • G banding: produced by staining with Giemsa after digesting the chromosomes with trypsin • C banding: chromosomes are treated with acid and base, then stained with Giesma stain
Making a karyotype • Karyotypes are presented in a standard form. • First, the total number of chromsomes is given, followed by a comma and the sex chromosome constitution. • This shorthand description is followed by coding of any autosomal abnormalities.
Preparing a karyotype • Metaphase cells required • any population of dividing cells could be used. • Blood, cultured skin fibroblasts, bone marrow cells. • lymphocytes induced to proliferate • many protocols but a standard series of steps is involved
Karyotype protocol • blood + heparin to prevent coagulation • centrifugation through dense medium: red cells and granulocytes pellet, no mononuclear cells (lymphocytes and monocytes). • cultured for 3-4 days in (mitogen) phytohemagglutinin, which stimulates proliferation. • add colcemid- disrupts mitotic spindles and prevents completion of mitosis. • harvested and treated with hypotonic solution: nuclei swell osmotically, aids good spreads • cells are fixed, put onto a slide and dried. • stained to induce a banding pattern
Diagnosis of abnormalities • Several metaphases are processed to control for artifacts ie extra or missing chromosomes. • Diagnose cases of mosaicism • Abnormalities in peripheral blood may need to be confirmed in other tissues • Analysis of diseased tissues can provide useful information. • E.g evaluation of cancers
Ploidy • Euploidy: normal number of structurally normal chromosomes. • Euploid females have 46 chromosomes (44 autosomes and two X chromosomes), • Aneuploidy: less or more than the normal diploid number • Most frequently observed type of cytogenetic abnormality. • Aneuploidy is recognised as a small deviation from euploidy because major deviations are rarely compatible with survival
Most common aneuploidies are monosomy and trisomy • Monosomy: lack of one of a pair of chromosomes. • A common monosomy seen in many species is X chromosome monosomy, Turner's syndrome. • Monosomy is usually lethal • Trisomy: a specific instance of polysomy. • i.e. Down syndrome, three 21s. • Triploidy. • Three of every chromosome • 69 human chrs (3 haploid sets of 23), • Due to fertilisation by two sperm. • rare and such individuals are quite abnormal. • survivers likely to be mosaic,
Chromosome abnormalities • Deletions occurs when a chromosome breaks and a piece is lost. • Results in partial monosomy for that chromosome. • Chromosome inversion cn occur after a breakage • Chromosome fragment is inverted and rejoined not lost. • Unless the breakpoints disrupt an important gene, phenotype may be normal.
Chromosomal translocations • Translocations: chromosomes break and the fragments rejoin to other chromosomes. • Many structurally different types of translocations • No loss of genetic material but breakpoint can disrupt a critical gene or juxtapose pieces of two genes to create a fusion gene • Translocations cause reductions in fertility.
Reciprocal translocation • Two non-homologous chrs break and exchange fragments. • Balanced complement of chrs and normal phenotype • But subfertility due to problems in pairing/ segregation during meiosis. • Translocation chrs and their homologs form quadrivalents. • Formation of unbalanced gametes and offspring with unbalanced genomes – • often lethal • Some offspring are cytogenetically normal • Others carry the translocation of their parent • Translocations are thus heritable
Centric Fusions • Robertsonian translocation • The karyotype carrying a centric fusion has one less than the normal diploid number of chrs. • Centric fusions cause a mild reduction in fertility (5-15%), much less severe than in the case of reciprocal translocations. A centric fusion is a translocation in which the centromeres of two acrocentric chromosomes fuse to generate one large metacentric chromosome
Isochromosomes • A chromosome can split "the wrong way" in mitosis (or meiosis II) • Both long arms remain attached and move to one pole • Both short arms do likewise moving to the other pole. • Isochromosomesare simultaneously duplicated for the genes in the retained arm and deleted for the genes in the other. • The prognosis is poor except for iXq (isochromosome of the long arm of the X).
Ring chromosomes • Mutation removes both telomeres • Repaired by sealing the ends together forming a ring chromosome. • Deleted for genes at both ends of the chromosome. • The symtoms will depend on the extent of the deletion. • Ring chromosomes are mitotically stable.
Chromosome abnormalities animations http://www.tokyo-med.ac.jp/genet/cai-e.htm
Mosaic • An individual with more than one cytogenetically-distinct population of cells. • The fraction each genotype is variable • Large proportion of abnormal cells will manifest disease. • Small number of normal cells may prevent or reduce disease. • Most humans with Turner's syndrome (X chromosome monosomy) die prior to birth. • Many survivers are found to be mosaics with a substantial fraction of normal cells (e.g. 46 XX/45 XO mosaics).
X chromosome Mosaicism • X inactivation occurs randomly • Normal females have equal populations of two genetically different cell types (type of mosaic) • In half their cells, the paternal X is inactivated, and in the other half the maternal X chromosome is inactive. • Important biological and medical implications, particularly in X-linked genetic diseases.
Why are chromosome studies important? • Diseases caused by missing/additional parts of or whole chromosomes • Downs syndrome plus 21 • Cri du chat missing part of short arm chr 5 • Turners missing an X or Y chr
Chromosomal Disease • 1 in every 200 newborn children has a chromosomal abnormality. • Some are phenotypically normal, while others have manifestations of disease. • These children have ‘mild’ disorders compatible with survival to term. • Half spontaneously aborted first trimester fetuses are abnormal • In preimplantation embryos higher numbers of abnormalities are seen. • Some chromosomal abnormalities are never seen, because they are so profound
Causes of Chromosomal Disorders • Ionising radiation, autoimmunity, virus infections and chemical toxins in the pathogenesis of certain disorders. • Most cases of simple aneuploidy - monosomy or trisomy - are likely due to meiotic non-disjunctions
Clinical presentation suggestive of chromosomal abnormality • Infertility and sterility: Cytogenetic analysis of such individuals is often warranted • Intersexes: genetic and phenotypic sex do not correspond. • Multiple congenital malformations: seen with many types of chromosomal abnormalities, particularly deletions and aneuploidy. • Mental retardation: Well-known examples of this are Down and fragile X syndromes.
Prenatal diagnosis • Amniocentesis:12 - 14 weeks of gestation fetal cells from amniotic fluid is drawn off.. • Chorionic villus sampling: 9-10 gestation, placental tissue aspirated via the cervix, • A single cell from an 8 cell stage embryo can be examined directly - used to decide on which embryo to reintroduce into the mother.
How are abnormalities diagnosed? • Normal karyotype • Down syndrome karyotype
FISH good at identifying abnormallities • Determines trisomies and monosomies. • probes for specific regions determine deletions, translocations, or duplications • trisomy 21 (right), • a probe for chromosome 22 detected a translocation, to chromosome 9 (left)
FISH technique • DNA probes are specific to regions of individual chrs. • Probe attaches to the spread of chrs • a fluorescein stain is applied. • visible with the aid of a fluorescent microscope. • The chr 21 pair have been painted.
Fluorescent in situ hybridisation • The tyramide signal amplification technology uses a fluorescent tyramide and HRP • Probe is labeled with biotin and detected by streptavidin-HRP or an antibody. • HRP reacts with a fluorescent tyramide in the presence of hydrogen peroxide to produce a reactive tyramide that attaches to proteins in the area. • The turnover of multiple dye-labeled tyramide substrates per peroxidase label results in strong signal amplification.
Metaphase FISH • Detect microdeletions beyond resolution of routine cytogenetics • Identify extra material of unknown origin. • Determine a simple deletion or a subtle or complex rearrangement. • Detect specific rearrangements in certain cancers. • Number of microdeletion syndromes diagnosed by FISH is expanding rapidly. • Probe may be specific for the gene as in Williams Syndrome • a deletion has been shown in the elastin gene in 96% of individuals with a firm diagnosis.
Cri-du-Chat Miller-Dieker Syndrome Smith-Magenis Syndrome Steroid Sulfatase Deficiency DiGeorge/Velo-Cardio-Facial/CATCH-22/Shprintzen Syndrome Kallman Syndrome Williams Syndrome Wolf-Hirschhorn Prader-Willi/Angelman Syndrome Microdeletion Syndromes Currently Diagnosable with FISH
Interphase FISH • Determine the chr number • Specific rearrangements in certain cancers. • Advantage is that it is rapid • Aneuploid Screen on amniotic fluid cells • Nuclei denatured and hybridized with probes for chromosomes 13, 18, 21, X, and Y and results usually obtained within 24 hours. • Routine cytogenetics is included to confirm the results or detect any abnormalities not detected by interphase FISH.
Aneuploid Screen test: Interphase FISH • Top nucleus chr 13 (green), and 21 (red). • Bottom nucleus probed for chromosomes 18 (aqua), X (green), and Y (red). • two signals each for chrs 13, 18, and 21 and one signal each for the X and Y • fetus is normal male with respect to the Aneuploid Screen test.
Metaphase cell • probed for DiGeorge/Velo-Cardio-Facial/CATCH 22/Shprintzen Syndrome • caused bymicrodeletion on chr 22. • dual-color mixture of two probes • Green- an internal control at 22q13. • red -at the DiGeorge region 22q11.2. • this individual would not have DiGeorge Syndrome.
Did chr 4 have a small terminal deletion at 4q? • or was there a more complex rearrangement? • Top:hybridized with a "painting" probe for chr 4 • Bottom:hybridized with a probe for 4q ter • only one green signal this confirms that one chr 4 is missing material from t 4qter • example of routine Cytogenetics and FISH can be used together
Steroid Sulfatase Deficiency • caused by a microdeletion on the X • two probes for the X chromosome, both red in color. • "X cen" control located at the X centromere. • "Xp22.3" probe is for the Steroid Sulfatase region at Xp22.3. • this is a female carrier for Steroid Sulfatase Deficiency.
Multicolour FISH • Can use probes of different colours to identify different all chromosomes at once • Chromosome rearrangement in an oral cancer cell shown with multi-colored painting probes.
BAC to paint • Research application • Chromosome breakpoints identified by our technique of paint-assisted microdissection fluorescence in situ hybridisation (PAM-FISH, at left) • breakpoints are mapped in greater detail using bacterial artificial chromosome FISH (BAC-FISH, at right)
Microarray/biochip-based technologies • In cytogenetics, promises to speed up detection of aberrations now detected by FISH. • Whole genome expression array and direct molecular analysis without amplification. • Analysis of single-cell gene expression promises a more precise understanding of human disease pathogenesis and has important diagnostic applications. • Optical Mapping can survey entire human genomes for insertions/deletions, • which account for more variation between closely-related genomes than SNPs • major cause of gene defects.
Molecular imaging technologies • Optical imaging, magnetic resonance imaging (MRI) and nuclear medicine techniques. • Positron emission tomography (PET)- technique for imaging molecular pathways in vivo in humans. • Cytogenetics refined by nanotechnological applications at single molecule level i.e single molecule imaging. • Atomic force microscope (AFM) is well-established for imaging single biomolecules under physiological conditions. • Scanning probe microscope (SPM) is important for non-intrusive interrogation of biomolecular systems in vitro and have been applied to improve FISH. • QD (quantum dot)-FISH probes, which can detect down to the single molecule level.
Why Do We Need Array CGH? • Current cytogenetic genome screen - karyotyping - even the best has low resolution (5MB) • FISH – better resolution (3MB), but only targeted regions • Molecular techniques - struggle with larger sized fragments and whole genome analysis
CGH BAC Micoarray – How Does it Work? Reference DNA Labeled with Cy5 (Detected with Red Laser) Patient DNA Labeled with Cy3 (Detected with Green Laser) + Cot-1 DNA Unlabeled + Glass slide spotted with DNA from known locations in the Genome
pter qter Cy3/Cy5 Ratios Test Sample Test Reference Test Cy5 Cy5 Cy3 Exp. 1 Exp. 2
The Scanner Images the Array Cy3 Image using a green laser Cy5 Image using a red laser
Reading a CGH-Microarray The resulting “colour” of a spot will depend on the ratio of “Red” and “Green” labeled DNA which has Hybridized to the Spot Equal Loss of patient DNA (Deletion) Excess Patient DNA (Duplication)
Composite Image of Individual Block Detail of array showing a possible deletion