Pharynx
790 likes | 1.59k Vues
Pharynx. By Dr. Nourizadeh Assistant professor of E.N.T. Anatomy. The pharynx is a musculomembranous tube that extends from the base of the skull to the level of the sixth cervical vertebra. The pharynx forms from the elongation and growth of the primitive foregut . . Anatomy.

Pharynx
E N D
Presentation Transcript
Pharynx By Dr. Nourizadeh Assistant professor of E.N.T
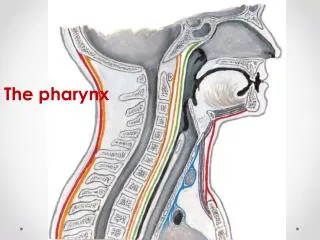
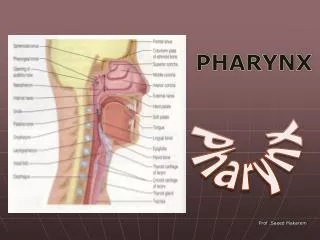
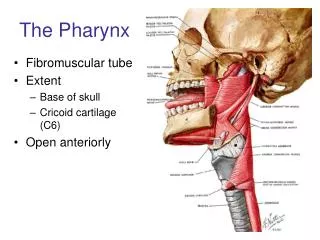
Anatomy • The pharynx is a musculomembranous tube that extends from the base of the skull to the level of the sixth cervical vertebra. • The pharynx forms from the elongation and growth of the primitive foregut.
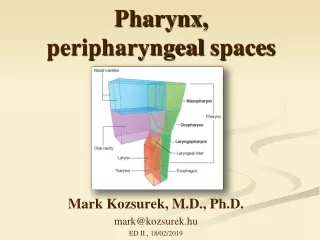
Anatomy • The mucosal lining of the oropharynx and hypopharynx is a nonkeratinizing stratified squamous epithelium that is tightly adherent to an underlying layer of fascia called the pharyngobasilar fascia. • The pharynx is surrounded by three constrictor muscles-the superior, middle, and inferior constrictors . • The pharyngeal muscles are enclosed by the buccopharyngeal or visceral fascia. Areas of loose connective tissue surround the visceral fascia of the pharynx and are potential spaces for infection.
Mucous membrane of nasopharynx Mucous membrane of oral pharynx Superior constrictor Middle constrictor Mucous membrane of laryngeal pharynx Inferior constrictor Esophagus
THE TONSILS • Waldeyer's ring is a continuous band of lymphoid tissue that surrounds the upper pharynx. • The superior portion of the ring is located in the nasopharynx and is composed of the adenoids. Laterally the palatine tonsils and anteriorly the lingual tonsils complete the ring. • Tonsillar crypts extend deeply into the body of the tonsil and are surrounded by lymphoid nodules. Debris and foreign particles collect within the crypts. • Theepithelium of the tonsils also varies by location. While the pharyngeal tonsil is covered mainly by multiple rows of ciliated epithelium, the palatine and lingual tonsils are covered by stratified, non-keratinized squamous epithelium.
The primary follicles are formed during embryonic development and differentiate into secondary follicles after birth. • The secondary follicles mainly contain B lymphocytes at various stages of differentiation, along with scattered T lymphocytes. • Tonsillar tumors or infections may result in ear pain due to referred pain conducted by cranial nerve IX.
The lymphatic tissue in the tonsillar ring is also termed the mucosa-associated lymphatic tissue (MALT) of the upper respiratory tract. • Active phase lasts until 8-10 years of age. • This function should not alter the decision to remove the tonsils if a valid indication for tonsillectomy exists.
TONGUE BASE • The sulcus terminalis, just posterior to the circumvallate papillae, divides the anterior twothirds of the tongue from the posterior oropharyngeal portion. • The hypoglossal nerve provides motor innervation. • Taste from the posterior tongue is mediated by the glossopharyngeal nerve. The lingual artery provides an abundant arterial supply.
Hypopharynx • It is subdivided into: • Pyriform sinus • Posterior pharyngeal wall • Postcricoid region • The glossopharyngeal and vagus nerves form a plexus that provides the motor and sensory innervation to the hypopharynx. • Additionally, the vagal innervation to the pyriform sinus frequently results in referred pain to the ear mediated via Arnold's nerve.
In performing the head and neck examination, it is crucial to palpate the oral cavity and oropharynx, as tumors , can be palpable with only subtle surface abnormalities.
Radiology • For a suspected retropharyngeal abscess, a lateral neck film can reveal thickening anterior to the vertebrae. • In general CT is preferable to magnetic resonance imaging (MRI) for its ability to better distinguish the tumor's relationship to osseous structures. MRI is particularly useful in evaluating tongue base lesions. • Barium swallow (Modified)
Throat Cultures: • At the initial presentation of tonsillitis, empiric antibiotic therapy is sufficient and cultures are not cost effective. • If the patient fails to respond to the antibiotic or the infection recurs soon after, a culture may be useful in directing future therapy. • Polysomnography: Airflow Oxygen saturation Electroencephalogram Rib cage and abdominal effort Esophageal pressure EKG
Infectious Disorders • The most common diseases of the oropharynx are inflammatory processes. • Pharyngitis is more common in children & adolescents than in adults. • In children, pharyngitis is most common after the age of 6 months. • Presents initially with high fever and severe pain on swallowing, which often radiates to the ear. Other symptoms are swollen tonsillar lymph nodes and muffling of speech due to oropharyngeal swelling.
Bacterial Adenotonsillitis • On examination, the tonsils are red and swollen, often contacting each other in the midline with yellowish or white spots or vesicles formed on them. • Malodorous breath can also accompany this disorder. • The most common bacterial causes of acute pharyngitis/tonsillitis: • Staphylococcus aureus • Group A hemolytic streptococcus • Haemophilusinfluenzae
The treatment of acute adenotonsillitis includes: • Increased oral intake • Bed rest • Analgesics • Antipyretic medications • The standard treatment for streptococcal tonsillitis is a 10–14 day course of penicillin V. • This regimen should be continued for at least 7 days to avoid late complications (see below). • Macrolides or oral Cephalosporins can be used in patients allergic to penicillin. Analgesics are also administered for pain relief.
Asymptomatic patients with a positive rapid test should not be placed on antibiotics. Conversely, a culture should be taken in cases where there is clinical suspicion of streptococcal tonsillitis but the rapid test is negative.
Antibiotics are indicated, however, in cases where the offending organism is group A hemolytic streptococcus. • The purpose of antibiotic treatment in these cases is prevention of potential renal and cardiac sequelae. • In addition, treatment of strep tonsillitis • Shortens the length of the illness • Irradicates the streptococcus from the pharynx so the infection cannot be transmitted to others • Prevents possible suppurative complications • The drug of choice is penicillin (if the patient is not penicillin allergic) for a 10-day course. Erythromycin can be used as a second-line agent. Clindamycin can also be utilized in patients who are allergic to penicillin.
Another treatment option would be a first-generation cephalosporin. it is generally accepted that if the community failure rate with penicillin is less than 10%, penicillin should be the first-line treatment. • Complications: • Peritonsillar edema and airway obstruction leading to a peritonsillar abscess • Deep neck infection • Septicemia • Rheumatic fever • Glomerulonephritis • Lingual tonsillitis • Streptococcal gingivostomatitis
Scarlet Fever • Group A β-hemolytic Streptococci that produce the scarlet fever exotoxin. • Sign & symptoms: • A rash that begins on the trunk. (“perioral pallor”) • A bright red tongue with a glistening surface and hyperplastic papillae (“raspberry tongue”). (Pathognomonic feature) • The tonsils are greatly swollen with a deep red color. • An enanthema of the soft palate with hemorrhagic areas. • The diagnosis is established by: • The overall clinical picture + a positive rapid streptococcal test
Treatment • Medical therapy relies on penicillin, as in acute tonsillitis. • the oral cavity should be rinsed with mild antiseptic solutions • analgesics should be given for pain Complications: • Necrotizing scarlet fever tonsillitis • Septic complications • Extensive soft-tissue infections • Toxic-shock-like syndrome • Rheumatic fever • Diffuse hemorrhagic glomerulonephritis • Rheumatoid arthritis
Diphtheria • Corynebacterium diphtheriae(The incubation period is 1–5 days) • Transmition routes: • Droplet inhalation • Skin-to-skin contact • Pathogenesis? • Diphtheria is generally suspected if a dirty-gray membrane covers the tonsils, tonsillar pillars, soft palate, and uvula.
Two main forms are distinguished based on their clinical presentation: • Local, benign pharyngeal diphtheria • Primary toxic, malignant diphtheria • The disease begins with moderate fever and mild swallowing difficulties. The clinical picture becomes fully developed in approximately 24 hours, characterized by severe malaise, headache, and nausea. • The symptoms of this condition are generally mild but can progress to upper airway obstruction or cardiac toxicity.
Treatment • First, the patient should be isolated. • Diphtheria antitoxin (200– 1000 IU/kg body weight) should be administered by intravenous or intramuscular injection. • Allergy to the antitoxin should be excluded (with a skin test) before it is administered. • Penicillin g should also be administered.
Discharge from the hospital is contingent upon test results: three smears taken at 1-week intervals must all be negative. • Two percent of patients continue to carry the bacterium and should undergo tonsillectomy.
The treatment for diphtheria is generally considered an emergency, and antitoxins should be given within the first 48 hours of onset to be effective.
Tuberculosis • Very rare (0.2%) • Clinical manifestations: • Primary complex: A primary tuberculous complex in the tonsillar and cervical lymph-node region is most common in children who have become infected by drinking cow’s milk contaminated with tubercle bacilli. The primary complex in these cases consists of a typical ulcerative lesion of the oral mucosa and tonsil, associated with regional cervical lymphadenopathy.“cold abscesses” may form about the cervical spine.
Miliary tuberculosis: involvement of the oral mucosa can result from hematogenous spread, appearing as multiple pinhead-size papules, some hemorrhagic, that form on the oral mucosa. • Diagnosis: • The detection of acid-fast rods in smears, sputum, bronchial secretions, gastric juice, or biopsy material. • Biplane chest radiographs • Tuberculin skin test • Calcifications detected by ultrasound in enlarged cervical lymph nodes are pathognomonic for tuberculosis. • Cervical lymph-node biopsy
Infectious Mononucleosis • Synonyms: Pfeiffer’s glandular fever, kissing disease • It predominantly affects adolescents and young adults. The incubation period is 7–9 days. • The patient may present with fever, pharyngitis, cervical adenopathy, and splenomegaly. Other symptoms include malaise, sore throat, dysphagia and odynophagia. (tonsillitis as the initial or cardinal symptom) • Examination will reveal enlarged tonsils, often with a dirty-gray exudate. The soft palate may be edematous with petechiae. • The blood count initially shows leukopenia, followed later by leukocytosis (20,000/μL) with 80–90% atypical lymphocytes (lymphomonocytoid cells, Pfeiffer cells).
In mononucleosis, the white blood cell count is elevated to 10,000 to 15,000 with 50% or more lymphocytes, which are atypical in structure. • EBV serology (especially IgM and IgG) is another important test. (ELISA) • The serum hepatic enzymes should be determined to exclude concomitant involvement of the liver or spleen. • Upper abdominal ultrasound and an electrocardiogram are also recommended. • Treatment is supportive, including bed rest, until the fever has resolved, with a gradual return to physical activity.
The agents of choice for pain relief are acetaminophen or ibuprofen. Aspirin products should not be used, as they could cause bleeding problems if tonsillectomy is required. • Ampicillin and Amoxicillin should be avoided because they frequently induce a pseudoallergic rash. • Care must be taken in patients with splenomegaly to avoid physical activity.
Rarely, hospital admission is required due to tonsillar hypertrophy and airway obstruction. In these cases monitoring for potential airway obstruction is appropriate, and corticosteroids may be of use. • If the severity of airway obstruction is significant and/or the airway obstruction fails to resolve with supportive care and corticosteroids, tonsillectomy and/or adenoidectomy may be warranted.
Peritonsillar Abscess (Quinsy) • Peritonsillar abscesses usually occur in patients with recurrent tonsillitis or those with chronic tonsillitis that has been inadequately treated. the absence of any history of tonsillitis is not uncommon. • This disease process is more common in young adults. Usually the process begins with a peritonsillarcellulitis that progresses into an abscess that extends beyond the tonsillar capsule. The abscess forms in the potential space between the buccopharyngeal fascia and the capsule itself. Abscess within the body of the tonsil itself is actually rare. • The swelling usually causes edema of the soft palate and displaces the tonsil medially forward and downward. This generally causes deviation of the uvula to the normal side.
Patients generally complain of extreme unilateral soreness of the throat with odynophagia, drooling, and trismus. Otalgia on the side of the infection is not uncommon. • Because it can be difficult at times to differentiate a peritonsillarcellulitis from a true abscess, some opt to initially treat with 24 hours of intrayenous antibiotics and hydration. If the patient improves during this time, the infection is most likely a cellulitis that will probably continue to improve with parental antibiotics. • Bearing in mind that most patients harbor a mixed spectrum of aerobic and anaerobic organisms.
Treatment: • Incision and drainage • Tonsillectomy • Intravenous antibiotics (Penicillin or Clindamycin) • Hydration • Analgesic
Retropharyngeal Space Infection • The retropharyngeal space lies behind the pharynx and esophagus, just anterior to the prevertebral fascia. It extends superiorly to the base of the skull and inferiorly to the bifurcation of the trachea. • Patients generally present with trismus, drooling, dyspnea, dysphagia, and a mass, often fluctuant, on one side of the posterior pharyngeal wall. • Lateral radiographs of the neck are also helpful in diagnosis. It is important, however, to have proper positioning of the patient at the time of X-ray; otherwise the results may be misleading. The patient should have the neck extended in a true lateral position for the X-ray.
A more sensitive evaluation is through a computed tomography scan of the retropharynx. A ring-enhanced lesion in this area is suggestive of an abscess. The presence of air within the lesion confirms that an abscess is present. • Once an abscess is diagnosed or suspected, either by air within the area of swelling, by CT scan evaluation, or by failure to improve on antibiotics a drainage procedure in the operating room is required. This is performed under general anesthesia.
Cortisone should also be administered in patients with significant dyspnea.
Parapharyngeal Space Abscess • The parapharyngeal space is cone shaped. Superiorly it starts at the base of the skull and inferiorly its margin ends at the hyoid bone. The superior constrictor muscle is the medial boundary, and the parotid gland, the mandible, and the pterygoid muscle are its lateral margins , the prevertebral fascia is present posteriorly. • A parapharyngeal space abscess can develop when infection or pus from the tonsillar region goes through the superior constrictor muscle. The abscess then forms between the superior constrictor muscle and deep cervical fascia. • Patients can present with toxemia and pain in the throat and neck, with tender swelling of the neck in the region of the angle of the mandible. Examination may reveal tonsillitis and/or medial displacement of the tonsil.
Trismus may also be present due to inflammation and edema around the pterygoid musculature. If only the posterior compartment is involved, there may be no trismus, but rather swelling of the lateral pharyngeal wall and perhaps of the posterior tonsillar pillar. This condition is best diagnosed by CT scan. • Once a parapharyngeal abscess is identified it needs to be surgically drained.
Foreign body The foreign material should be removed as soon as possible due to the risk of superinfection.
NEOPLASMS • The overwhelming majority of malignant tumors of the oropharynx are squamous cell carcinomas. • Approximately 80% are located in the palatine tonsils or tongue base. • Less common sites are the soft palate and posterior wall of the pharynx. • In most patients, chronic nicotine and alcohol abuse have a major etiologic role in the development of oropharyngeal cancers.
Lymphoma • The lymphomas occur most commonly in the tonsil where they represent 16% of all neoplasms. • Lymphomas can occur anywhere in Waldeyer's ring, and are almost always non-Hodgkin's lymphomas. • Treatment is primarily nonsurgical.