Understanding Acute Limb Ischemia: Causes, Symptoms, and Emergency Management
740 likes | 1.02k Vues
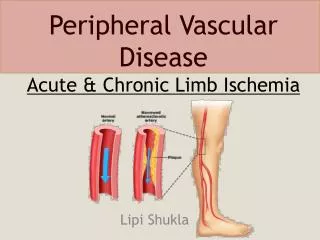
Acute Limb Ischemia (ALI) is characterized by a sudden decrease or worsening of limb perfusion, posing a threat to extremity mobility and viability, typically within 14 days. Prompt diagnosis and restoration of blood flow are crucial to prevent irreversible tissue loss. The primary causes include embolism, thrombosis, and trauma, particularly arising from cardiac sources. Clinical indicators include severe pain, paresthesias, pallor, and paralysis. Effective management involves timely interventions, including medication and possibly surgical revascularization, to restore blood flow and prevent complications.

Understanding Acute Limb Ischemia: Causes, Symptoms, and Emergency Management
E N D
Presentation Transcript
Acute Limb Ischemia: • sudden decrease in or worsening of limp perfusion causing a thread to extremity mobility and viability that has been present for less than 14 days. • There is no time for collaterals to form. • may lead to irreversible tissue loss within hours if rapid diagnosis and restoration of flow are not achieved.
Etiology: • Embolism * (the most common) • Thrombsis • Trauma • Iatrogenic
Embolism • Translocation of material within the arterial stream to a more distal site. • 80% of the emboli are cardiac in origin • Or it may come from an Aneurysm • OrAtherosclerotic plaques. • Usually lodges at site of bifurication , most commonly the femoral artery . Sources of emboli:
Cardiac pathology. 80% • Atrial thrombus. (atrial fibrillation – atrial cardiac myxoma) • Ventricular thrombus. (following MI – ventricular aneurism) • Damaged valves . (RHD produce microemboli) • Patent foramen ovale. (allow paradoxical embolism to travel from venous into arterial circulation)
Proximal arterial pathology : (arterial –arterial embolism) • Aneurysm (most commonly the infrarenal aorta or popliteal arteries – may harbor a mural thrompus) • Atherosclerotic plaques. (serve as a nidus for thrombus or platelet aggregate that embolize distally – rupture discharging small debris.
In situ thrombosis: • Thrombosis of a chronically diseased vessel (most commonly SFA and popliteal A- may cause acute ischemia if collateral circulation is poorly developed ) • Hypercoagulable states .(even if the arterial segment is normal – generally occurs in the more distal segments such as tibial vessels or pedal arches)
Clinical presentation: • The “6 Ps” define this syndrome: • Paresthesias . The 1st to appear. (sever neural dysfunction –herald impending limp loss –an insensate limp is generally considered nonviable • Pain(acute onset – severe – unremitting-mainly unilateral ) • Pallor(associated with coolness – occurs at one level below the occlusion) • Poikilothermia(coldness). • Plusless( and usually will not have detectable Doppler signals distally because their collaterals may not be developed enough to support distal flow. • Paralysis(result as muscle function is severely compromised – heralds limp loss if blood flow is not restored promptly)
How to mange this patient: • History: • Pain: onset, location, duration • Hx of previous claudication • Hx of cardiac disease: valvular HD, atrial fibrillation, MI * (the commenestptn. of acute limb ischemia) ,cardiomyopathy • Hx of recent trauma • Risk factors of cardiovascular disease: (HTN – DM – hyperlipidemia – smoking – family history)
Physical examination: • Compare with contralateral extremity involving: • Level of pulslesness . • Temperature . • Mottling . • Motor and sensory examination • Cardiac Ex :rhythm , murmurs
Investigations: • Non invasive examinations: • Doppler signals . Other non invasive Ex generally are not performed at the interest of time. • Invasive procedures : - Arteriography : to define the level of occlusion and distal reconstitution.
Treatment : • Goals : rapid restoration of blood in order to save the limb , but not on expense of life. Strategies: • ABCs • Heparin: to prevent further propagation of the thrombus. • Thrombolytic therapy in selected patients. • Rapid surgical restoration(revascularaization) : thrombectomy.
Heparin therapy : initial therapy for patient with AAI, unless there is contraindication – 100 u/kg bolus then continued empirically at 1000 u/hr up to the time of surgery • Hydration :to maintain adequate urine output . Alklinazation of urine and osmotic diuresis are used to protect the kidney from damage by myoglobinuria in patient with prolonged sever ischemia
Revascularization : Definite treatment – ideally is performed within 6h of the onset to avoid irreparable nerve and muscle damage. Surgical therapy :the patient should be taken directly to OR following heparinization especially if motor and sensory changes are present. • Embolectomy (the procedure of choice for macroembolism to a large artery) • Bypass ( thrombosis – when adequate thromboembolectomy can not be performed)
Thrombolytic therapy: In selected patients such as those with prior vascular intervention. Tissue plasmiogen activator and urokinase have been used to dissolve acutely formed thrombus. Contraindications include : Prescience of sensory and motor changes on presentation (it requires 24h of treatment Recent surgery Known intracranial pathology
Complication of revascularization: Reperfusion injury, which has two effects: • local effect : compartment syndrome . For that reason ,fasciotomy is done with thrombectomy as prophylactic. • Systemic effect: release of K & myoglobin. This will lead to cardiac arrest & ARF.
Compartment syndrome: Reperfusion injery to the muscle may result in swelling and increased compartment pressure within the facial spaces of the calf . Pathophysiology: Endothelial cell injury during ischemia capillary permeability and edema Tissue swelling after reperfusion intracompartment pressure (more than capillary perfusion pressure – 30 mmhg) decrease perfusion Ischemia and myonecrosis
Clinical features: Pain :after passive movement of the foot Paralysis Parasthesia Pallor Pulse usualy present Diagnosis: History Suspicion Measuring compartment pressure
Management : • Prevention : low threshould for faciotomy • Treatment : opening compartments via bilateral calf incision
What is ulcer ? • Ulcer is a break through an epithelial surface .
Types of lower limb ulceration : Iatrogenic Bandaging ,Casts Neoplastic 2% BCC , SCC Melanoma Marjolin’s Lymphoedema Traumatic Vasculitic RA ,PAN Metabolic Pyodermagangrenosum Pretibialmyxoedema Cryopathic • Vascular *** • Venous 70% • Arterial 10% • Mixed 10% • Neuropathic • DM • Alcohol • Spina bifida • Infective • Fungal • TB • Syphilis • Leprosy
Venous ulcer : • The most common cause of leg ulceration is venous disease . • Two third of all leg ulcers are caused by venous disease. Pathophysiology: • Reflux (90%) • Obstruction (10%)
Pathophysiology: • Reflux of venous blood will lead to venous hypertention • This in turn leads to edema and leakage of blood cells and fibrin into the tissues • This will cause discoloration and hardening of the tissues (lipodermatoscelerosis) • These tissues are then prone to injury
Valvular incompetence resulting in reflux may occur in either : - spuerficial veins resulting in varicose veins , or - deep veins (e.g. DVT is a cause of deep vein incompetence)
Causes of obstruction : • Pregnancy • Fibroids/ovarian cysts • Abdominal lymphadenopathy • Pelvic cancer • Iliac vein thrombosis
Evaluation • History • Physical Examination • Investigations Non-invasive (Doppler/Duplex) Invasive ( Venography)
History • History : age , sex, occupation • History of leg ulcer : duration , No. of ulcers or episodes , pain, discharge • Vascular history: Hx of DVT, venous surgery, sclerotherapy , Hx of claudication and IHD, CVA ...
Examination Local : • The leg: varicose veins , arteries and nerves • the ulcer: site ( gaiter area = above the medial malleolus), shape , size, edge (sloping), base ( usually covered with granulation tissue, depth ( usually shallow), discharge. • the surrounding tissues : usually show signs of chronic venous hypertentsion – induration and pigmentation, warmth, redness, tenderness. General : examine the abdomen, the other leg , local lymph nodes
Investigations • Non-invasive : Doppler ( augmentation, phasic movement), ABI (Ankle-Brachial Index) Duplex ( compressibility, valve incompetence) • Invasive : venogram
Keys to management: • Elevation of Feet at right atrial level • Dressings • Compression • +/- surgery
Management • In patient with venous ulcer due to superficial incompetence varicose vein surgery is effective . • In deep venous incompetence : - local ulcer management - application of compression
Local ulcer management • Clean the ulcer by soaking it in tap water • Debride the ulcer to remove any slough • no role for topical antibiotics or topical drugs to speed the healing • The most important factor in achieving healing is the use of high levels of compression
Compression • Dressing alone is not enough • It has been found that pressures of 30-45 mmHg applied to the ulcer are much more effective than lower level of compression • These can be achieved by - Compression stocking or by bandaging ( e.g. four-layer bandaging technique)
Sclerotherapy, • endovenous laser therapy (EVLT), endovenous ablation therapy and • surgery are other option to treat the underlying cause.
Neuropathic ulcer • Occur over pressure areas • Usually are deep penetrating ulcers • The surrounding tissues are healthy and have a good circulation • Painless
Diabetic Neuropathic ulcer It result from a combination of factors • peripheral polyneuropathy • ischemic changes due to arterial disease • retardation of wound healing • infection
Management General measures : • control diabetes • stop smoking • lose weight • refer to chiropodist Local : • Treat infection with antibiotics • Antiseptic and dressings • Remove necrotic tissues • Amputations with debridement of dead tissues until healthy bleeding tissue is obtained
Malignant ulcers: • BCC • SCC • Melanoma • Marjolin’s