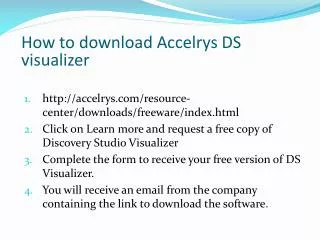
How to download Accelrys DS visualizer
270 likes | 589 Vues
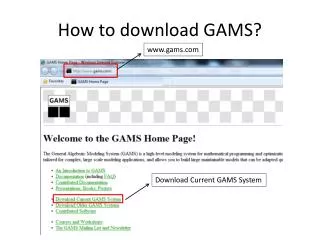
How to download Accelrys DS visualizer. http://accelrys.com/resource-center/downloads/freeware/index.html Click on Learn more and request a free copy of Discovery Studio Visualizer Complete the form to receive your free version of DS Visualizer.

How to download Accelrys DS visualizer
E N D
Presentation Transcript
How to download Accelrys DS visualizer • http://accelrys.com/resource-center/downloads/freeware/index.html • Click on Learn more and request a free copy of Discovery Studio Visualizer • Complete the form to receive your free version of DS Visualizer. • You will receive an email from the company containing the link to download the software.
Chloramphenicol • First, isolated from streptomyces bacteria in 1947. • Due to its simple structure, nowadays it is widely produced in large scale by chemical synthesis from P-nitroacetophenone. • It has a bacteriostatic action, inhibiting bacterial protein biosynthesis…. Believed to be through inhibiting the elongation step. • It has a broad spectrum of activity, but because of its serious systemic toxicity (aplastic anemia), it is mainly used topically for skin and eye infections.
Chloramphenicol • Active on both gram +ve and gram –ve bacteria, even on penicillin resistant strains such as H.influenza, N. meningititisand S. pneumonia. • It has a good penetration to CNS… used in meningitis. • Not recommended in UTI (why?)… only 5-10% of the unmetabolizedchloramphenicol is excreted in urine. • Bacteria became resistant to chloramphenicol through the production of chloramphenicolacyltransferase which acylate the OH group at C1 and C3 to the inactive esters.
SAR of Chloramphenicol • P-nitro group can be replaced by other aryl ring or oxygenated functional group without great loss in activity. • Phenyl ring can accept multi-substitutions. • Conversions of 1-OH to keto group causes appreciable loss inactivity.
Chloramphenicol esters • They have better physicochemical properties than Chloramphenicol which has both bitter taste and bad water solubility.
Quinolones antibacterial agents • Nalidixic acid is the lead compound for this group. • According to the heterocyclic core can be divided into: • Naphthyridines: nalidixic acid and enoxacin. • Quinolines: norfloxacin, ciprofloxacin, ofloxacin, lemofloxacin. • Cinnolines: Cinoxacin
Quinolones antibacterial agents • Spectrum of activity: • Highly active against urinary tract pathogens such as E. coli, Klebsiella, Citrobacter, proteusas well as salmonella and shigella. • Most except fluoroquinolones are not active on P. aeruginosa and H. influenza. • Inactive on anaerobic and gram +ve bacteria. • Pharmacokinetics: • They have good oral bioavailability. • They reach urine in enough concentration to be effective in UTI (>40%).
Quinolones antibacterial agents • Mechanism of action: Inhibit DNA synthesis by inhibiting DNA gyrase (topoisomerase-II) which is important for DNA supercoiling. • Transport into bacterial cell: mainly through the porin channels of the gram –ve bacteria. • Mechanisms of bacterial resistance: • Mutation in porin channels. • Energy dependant efflux mechanism.
SAR of Quinolones • The carboxylic acid at C3 is essential for activity. • Pyridone ring must be annulated with aromatic ring such as in Naphthyridine, Quinolines and Cinnolines. • Isosteric replacement of nitrogen for C2, C5, C6 or C8 resulted in retained activity. • Substitution at C2 greatly reduces or abolishes activity. • Positions 5,6,7 and 8 can be substituted for better efficacy
SAR of Quinolones • Positions 5,6,7 and 8 can be substituted for better efficacy: • Piperazine ring and 3-aminopyrrolidine at C7 enhances activity, mainly against P. aeruginosa. • Fluorine atom at C6 also improved activity (Fluoroquinolones). • Alkyl substitution on C1 improves activity (but small alkyl or aryl group). • Ring condensation at 1-8, 5-6, 6-7 and 7-8 also lead to better activity.
Fluoroquinolones • They are 6-fluoro-7-piperazinoquinolones derivatives. • They exhibit extended spectrum of activity that covers most of gram +ve and gram –ve bacteria especially P. aeruginosa. • Members: • Ciprofloxacin. • Norfloxacin. • Ofloxacin. • Pefloxacin. • Lomefloxacin. • Enofloxacin. • Levofloxacin.
Chemical structure of Fluoroquinolones • Have an acidic (3-carboxylic acid) and basic (piperazinyl) group, this makes these compounds present as zwitterionic species at physiological pH. • Like tetracyclines, they have chelating properties due to the presence of β-diketo structure. They can form stable, insoluble metal complexes with di and trivalent metal ions: • They should not be given along with antacids and mineral supplements. • formation of this chelate will reduce the oral availability of these agents.
Chemical structure of Fluoroquinolones • Fluorine atom at C6 increases potency against gram –ve bacteria. • The piperazinyl group at C7 improves anti-psuedomonal activity of Fluoroquinolones. • Chelation also has another –ve effect: the possibility to chelate with urine ions (Mg++ and Ca++) which leads to crystalluria Renal failure sometimes.
Ciprofloxacin Enoxacin • Well absorbed following oral administration (90%). • Well distributed through the body… reaches kidney, prostate and cervix. • Used mainly in prostatitis. • 40-50% excreted unchanged in urine. • Highly distributed to all body fluids including CS fluid. • Highly potent against gram –ve especially P. aeruginosa (why?). • Used in gastroenteritis, skin, soft tissues (bone and joints) infections and UTI.
Ofloxacin • Has 1,4-oxazine ring. • Has better penetration to CNS than ciprofloxacin (why?). • The structure has asymmetric carbon atom, normally ofloxacin is given as racemate, although the 3S(-) isomer is 125x more active than the 3R(+) isomer. • Recently the 3S(-) isomer (Levofloxacin) has been prepared and now marketed instead of ofloxacin which is more potent (Chiral switching phenomenon)
Lomefloxacin • Has longer duration of action (t1/2 =7-8hrs), this is believed to be due to: • Excellent tissue distribution. • Efficient renal reabsorption. • The only one that is given once daily. • It has an excellent oral bioavailability (98%). • Mainly used in acute bronchitis. • High incidence of phototoxicity due to the presence of two fluorine atoms. • Phototoxicity: is the formation of highly reactive oxygen radicals due to the exposure to light.
Sparfloxacillin • Higher potency against gram +ve Staphylococcus and streptococcus bacteria. • More active on anaerobic bacteria and Chlamydia. • Long t1/2 (= 18hrs) • Has the lowest incidence for phototoxicity.
New generation fluoroquinolones • Gemifloxacin: • is an oral broad-spectrum quinolone antibacterial agent. • Active against both gram +ve and gram –ve bacteria except P. aeruginosa. • used in the treatment of chronic bronchitis and mild-to-moderate pneumonia. • Has a protein binding of 60-70%. • Only 5-10% of the drug will be metabolized in the body to give the N-acetyl and the glucuronide conjugate.
New generation fluoroquinolones • Moxifloxacin: • Considered a fourth generation quinolones. • Given orally, parenterally and as eye drops for treatment of conjunctivitis (Bayer). • Uses: • Chronic bronchitis. • Acute bacterial sinusitis. • Pneumonia. • Skin infections. • 20% excreted unchanged in urine and 25% in feces. • More than 50% of the drug metabolized to the sulfate and glucuronide conjugates.