Lyme Disease
260 likes | 289 Vues
Learn who's at risk, preventive measures, tick removal, antibiotic therapy, reinfection possibility, and more about Lyme disease, its symptoms, and related tick-borne diseases.

Lyme Disease
E N D
Presentation Transcript
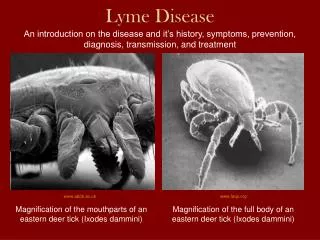
Who is at risk for Lyme disease? • People in areas with B. burgdorferi-infected ticks • In U.S., mostly northeastern, upper midwesternregions • Travelers to environments where ticks are present • Areas frequented by the animals that ticks feed on: birds, small mammals, deer • Wooded areas, areas with tall brush or grass • Under leaves, in wood piles
What protective clothing can be worn to prevent tick bites? • Long pants and long-sleeved shirts • Light-colored clothes (easier to spot crawling ticks) • Clothing impregnated with or sprayed with permethrin • Tuck pants into socks • Insect repellants containing DEET • Other insect repellants seem to be less effective
How should ticks be removed to reduce the chance of infection? • Just brush off ticks that have not attached • If ticks have attached to host: • Grasp tick at point nearest attachment site with flat tweezers or fingers, apply gentle, constant tugging • Mouthparts will release after about a minute • If residual mouthparts are left in skin, leave those alone • Mouthparts will extrude from skin naturally over time • Nightly “tick check” may reduce transmission • Takes 24-48 h for B. burgdorferi to move from tick to host
Should antibiotic therapy be given after a tick bite to prevent infection? • Single-dose doxycycline prophylaxis recommended if: • Ixodes adult or nymph has been attached for ≥36 h • Prophylaxis can be provided ≤72 h of tick removal • Local rate of B. burgdorferi infection in ticks >20% • Doxycycline can be used • Efficacy of prophylaxis unknown in children >8 y (don’t use doxycycline for children ≤8 y) • Alternative: watch for EM, other signs of infection • Initiate treatment if they develop Lyme disease • Outcomes excellent if treated during early EM stage
Is it possible to acquire Lyme disease more than once? • Patients treated early in disease can be reinfected • Antibodies are not protective • Antibodies offer only strain-specific protection • Patients with late-stage manifestations unlikely to be reinfected • Have broad antibody responses to multiple antigens • Patients with frequent tick bites may develop immune responses manifested by itching at the bite site
Should preexposure antibiotic prophylaxis ever be used? Is there a vaccine? • No studies support preexposure prophylaxis • Human vaccine previously approved in the U.S. • Utilized outer surface protein A of B. burgdorferi as antigen • Withdrawn in 2002 due to low sales • Available for dogs
CLINICAL BOTTOM LINE: Prevention... • Tick avoidance is the mainstay of prevention • To decrease transmission: use repellants, insecticides, and change behavior (wear protective clothing) • Spray acaricides to kill ticks around houses • Little evidence that these practices prevent of Lyme disease
What symptoms and signs should prompt investigation for Lyme disease? • Risk factor for tick exposure • Living in or frequenting endemic areas • Symptoms consistent with Lyme disease • Fever, fatigue and/or malaise, headache, arthralgia, myalgia, articular articular inflammatory arthritis • Erythema migrans • Carditis • Peripheral neuropathy • Encephalomyelitis • Many people are unaware of having been bitten
Early localized disease • 3-30 days after tick exposure • Characterized by EM at the site of the tick bite • Acute localized disease with systemic symptoms • Early disseminated disease • Days after original EM lesion to a month after tick exposure • Bacteria travel bloodstream to sites distant original EM • Secondary EM, acute carditis, nervous system symptoms, articular arthritis • Late disseminated Lyme disease • Months to years after the original tick exposure • Joint and/or nervous system symptoms • Other systemic symptoms are usually not present
What other diseases should be considered in a patient who becomes ill after a tick bite? • Patients may be co-infected with more than one agent • Ticks may be simultaneously infected • B. burgdorferi, Anaplasma phagocytophilum, Babesia microti, Borrelia miyamotoi • Other diseases transmitted by Ixodes ticks • Encephalitis virus (Europe) • Related Powassan virus called deer tick virus (U.S.) • Febrile illnesses without EM • Southern tick-associated rash illness transmitted by Amblyomma americanum ticks
What diagnostic tests should be done to confirm Lyme disease and other tick-borne diseases? • Testing is not always warranted • Do not test if patients in endemic areas and potentially exposed to ticks present with EM: treat with antibiotics • Do not test if patients in endemic areas have no history of tick exposure or only nonspecific symptoms • High incidence of false+ results associated with testing • Current testing recommendation is 2-step approach • Initial screening with ELISA • If positive, follow with supplemental Western blot test • Both tests can identify either IgM or IgG antibodies
Caveats to serologic testing • Sensitivity suboptimal during first 2 weeks of disease • Don’t order IgM testing in patients with >1 month symptoms (associated with more false-positive results) • Absence of positive results not evidence patient did not have disease (early antibiotic treatment abrogates results) • C6 antibody test: newer, first-step ELISA • Sensitivity equal to IgM ELISAs during early stages • Specificity is high but less than that of 2-step testing • More sensitive than 2-step testing for certain strains in early disease and for B. burgdorferi species in Europe • Testing for co-infection is routine in areas where rates are high
What are the major complications of Lyme disease, how often do they occur, and how should they be diagnosed? • Major manifestations usually resolve over time • EM, facial palsy, heart block, arthritis • Recovery typically complete except for nerve palsies and radiculopathy • Antibiotic therapy speeds resolution of some symptoms (arthritis, cardiac conduction delay), not all (facial palsy) • Treatment in early stages of disease generally results in excellent outcomes with minimal sequelae • Serologic testing used to assess probability of Lyme disease as cause of these symptoms (exception: EM)
Differential diagnoses for for the major manifestations of Lyme disease • Febrile viral illnesses • Facial nerve palsy • Viral meningitis • Heart block • Inflammatory arthritis • Peripheral neuropathy • Radiculoneuropathy • Encephalomyelitis • Cellulitis • Urticaria • Rocky mountain spotted fever • Cutaneous fungal infections • Local reaction to tick bites • Southern tick-associated rash illness
What is the role of a spinal tap in the evaluation of Lyme disease? • Studies of CSF can help establish neuroborreliosis • PCR: Very low sensitivity (0%-20%); don’t use routinely • Lyme CSF:serum antibody index • Sensitive and specific but often performed or ordered incorrectly • Standard ELISAs can’t be used • CSF evaluation can r/o other causes of disease in suspected Lyme disease with meningitis symptoms • In acute Lyme disease, CSF evaluation can guide choice of antibiotics
Is there any role for antibody screening to detect previous infection in asymptomatic persons? • Routine serologic screening of asymptomatic persons living in endemic areas is notrecommended • High number of false-positive results if used on population with low prior probability of disease • No studies support routine treatment of asymptomatic seropositive patients • Expert opinion is divided
CLINICAL BOTTOM LINE: Diagnosis... • With manifestations other than EM, diagnosis depends on serologic testing • Serologic testing more reliable for later-stage disease • Lower sensitivity in early disease • 2-step testing increases specificity, may decrease sensitivity • Use serologic results in conjunction with clinical and epidemiologic data to make diagnosis
What antibiotic treatment should be given? For how long? • Efficacy equal: penicillins, tetracyclines, some 2nd and 3rd generation cephalosporins • Macrolides may be less efficacious • Doxycycline has best bioavailability, CNS penetration • Minocycline also good oral bioavailability, CNS penetration but associated with vestibular side effects • Consider stage of disease and organs involved • Determines oral vs parenteral therapy • Determines treatment duration
Localized disease: oral antibiotics (i.e., doxycycline 100 mg orally twice daily for 10-21 days) • Early disseminated disease (mild carditis, isolated facial nerve palsy): extend oral regimen to 21-28 days • Higher degree heart block or meningitis: parenteral therapy with ceftriaxone 2 g IV once daily • Severe neurologic disease: full course of parenteral therapy • Late-stage arthritis: oral antibiotics for 28 days; consider second course (oral or parenteral) if arthritis continues • Pregnant women: don’t use doxycycline • Children: use adjusted dosages and don’t use doxycycline if younger than 8 y old
When should a patient with suspected or confirmed Lyme disease be admitted to the hospital? • Hospitalize patients with high-degree heart block • Required for management • Consider hospitalizing patients with meningitis, arthritis • To establish diagnosis, determine Lyme disease as cause • Consider hospitalizing patients when initiating parenteral therapy
How should cardiac complications of Lyme disease be treated? • Atrioventricular conduction delays range from first-degree to complete heart block • Administer antibiotics as soon as diagnosis established • Prior to confirmatory serologic testing if suspicion is high • Treat second- and third-degree heart block in hospital • Use IV antibiotics • Once heart block has resolved, switch to oral antibiotics • Temporary pacing device may be needed
How should the neurologic complications of Lyme disease be treated? • Treat isolated peripheral nerve facial palsy with oral antibiotics • Most patients with unilateral Lyme facial palsy recover fully • Some with bilateral facial palsy have residual deficits • For patients with involvement of other cranial nerves, parenteral antibiotics recommended
What is "chronic Lyme disease," and how should it be treated? • Continuation of symptoms after antibiotic therapy • Fatigue, myalgia, arthralgia, memory loss, headache • Long-term fibromyalgia- or chronic fatigue-like symptoms • Highly controversial whether legitimate clinical entity • Symptoms may occur at same rate as in general population • Current recommendation for management of chronic disease: supportive care only
“Chronic Lyme disease” distinguished from well-accepted Lyme disease sequelae • Little disagreement some manifestations persist after antibiotic therapy • Arthritis, neuropathy, radiculopathy • Can be documented objectively through medical testing • Persistent arthritis after antibiotic therapy often responds to anti-inflammatory or immunomodulatory agents • Possible mechanisms for persistent manifestations • Preexisting damage from inflammatory response to infection • Persistent low-level infection • Autoimmune response
CLINICAL BOTTOM LINE: Treatment... • Lyme disease symptoms resolve in most patients • Even without antibiotic therapy • Antibiotic therapy recommended • To hasten resolution of symptoms • To prevent late sequelae • First-line therapy for Lyme disease: oral antibiotics • Initiate parenteral therapy if severe cardiac or neurologic symptoms are present • Can likely switch to oral antibiotics as patient improves